Updating the stroke assessment
Direct percutaneous puncture of the cervical carotid artery remained the primary technique unto the 1960s to visualize intracranial blood vessels until Seldinger’s technique was introduced in 1953. This was a diagnostic procedure after the stroke or TIA (Varon, Varon, & Nyman, 2007)
I was employed as a Radiologic Technologist (X-ray tech) in the 1980s and 90s in the Cath lab and Interventional Radiology and we were doing cardiac procedures, angioplasty and stenting of coronary arteries. We had a Neuroradiologist performing the diagnostic angiography and I asked why aren’t we doing anything treatment wise for stroke patients. He gave a 3-part answer. First the imaging on the monitor was not accurate enough, think about your television at that time compared to today. Second the catheters weren’t small enough to access arteries in the brain. Third, he replied, I’m close to retirement, a lot of things can happen maneuvering catheters in a patient’s brain, some of them bad. You need a younger doctor with bigger cahoonas. Those three things have happened.
Since the 1970s Computerized axial tomography (CAT) and magnetic resonance imaging (MRI) replaced cerebral arteriography for localizing tumors and epidural or subdural hemorrhage, however, angiography is now used currently for embolization of aneurysms and removal of thrombi or emboli in patients with acute stroke.
The CPSS (Cincinnati Prehospital Stroke Scale) was derived from the National Institutes of Health Stroke Scale developed in 1997 at the University of Cincinnati Medical Center for prehospital use. Launched in late 1998, ASLS® (Advanced Stroke Life Support) is an 8-hour curriculum that addresses the prehospital, emergency department, and inpatient hospital management of patients with acute stroke, incorporating interactive discussions, hands-on workshops, video cases and standardized patient simulations. ASLS® was developed by the Michael S. Gordon Center for Research in Medical Education, a center of excellence at the Leonard Miller School of Medicine of the University of Miami. They have now partnered with the American Heart Association. ASLS compared to what we are doing now for patient assessment is like ACLS is to BLS. ASLS is not mentioned in the 2020 ACLS manual.
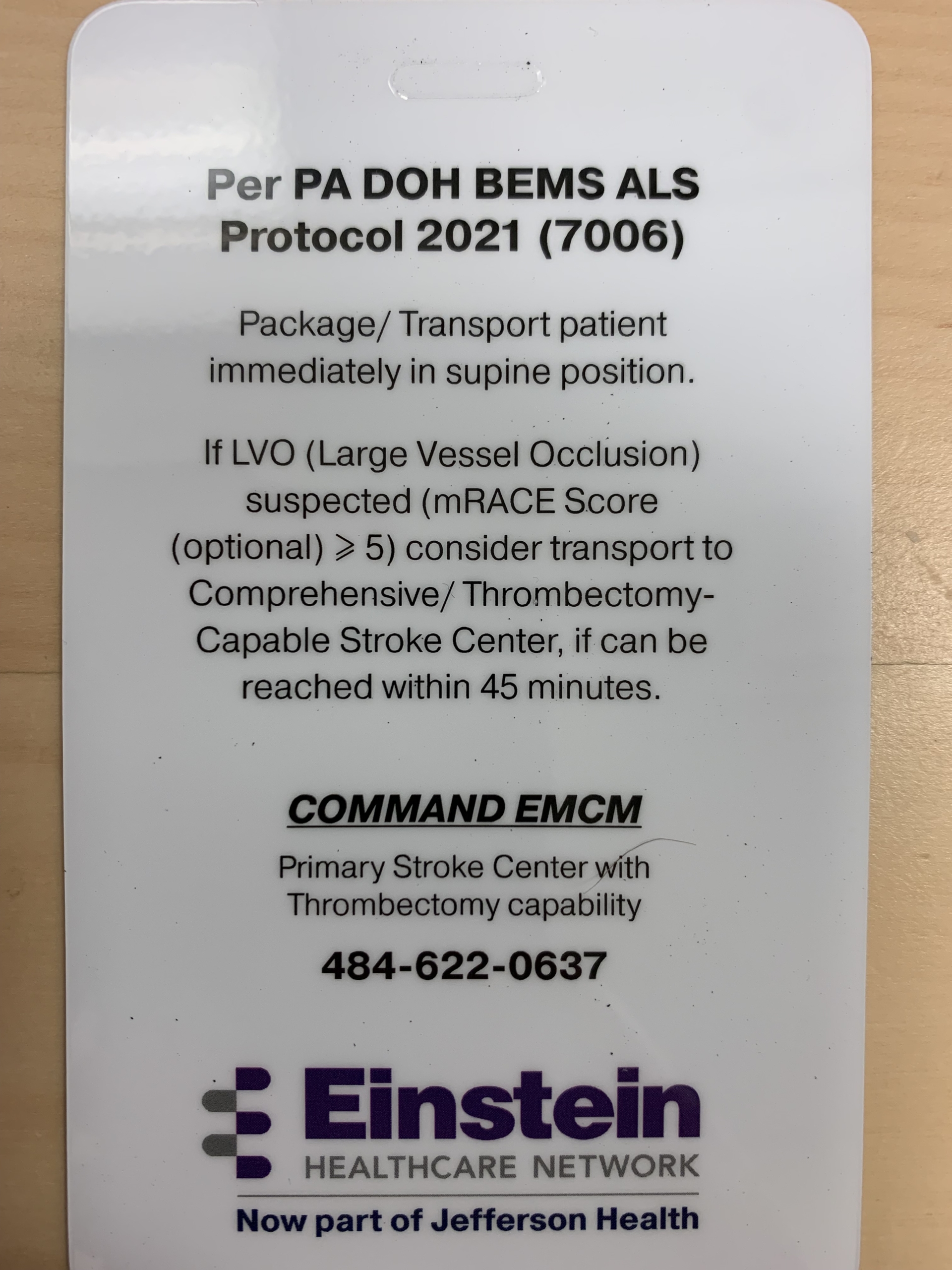
ASLS and other stroke assessments will provide a more accurate impression of where the patient’s problem is and where we transport them to for treatment.
Remember the circle of Willis? (Vrselja, Brkić, Mrdenovic, Radić, & Ćurić, 2014). Think of the circle of Willis as a beltway around a large city. Interstates and highways are the carotid and vertebral arteries feeding into the circle and the exits are smaller cerebral vessels throughout the brain. With more advanced patient assessments we can better locate the part of the brain involved; we might reach them with a catheter or stent retrieval system to remove an occlusive clot or repair an aneurysm. Similar to the 12-lead EKG pointing to a specific area of the heart, not just a 3-lead.
Bibliography
Varon, J., Varon, J., & Nyman, U. (2007). Sven-Ivar Seldinger: The revolution of radiology and acute intravascular access. Resuscitation, 75(1), 7-11. Retrieved 6 25, 2023, from https://ncbi.nlm.nih.gov/pubmed/17573177
Vrselja, Z., Brkić, H., Mrdenovic, S., Radić, R., & Ćurić, G. (2014). Function of circle of Willis. Journal of Cerebral Blood Flow and Metabolism, 34(4), 578-584. Retrieved 6 26, 2023, from https://ncbi.nlm.nih.gov/pmc/articles/pmc3982101
Cincinnati Prehospital Stroke Scale – Wikipedia.
Advanced Stroke Life Support
https://cpr.heart.org/en/private/asls-course