End-tidal carbon dioxide (ETCO2) has been around for a while now. We started with the main-stream (BVM/ ET tube attachment) that we can use on our mechanically ventilated patients, and then we progressed to having the side-stream (nasal cannula type device) that we can use on all of our breathing patients. End-tidal has become the gold standard for determining if our patients are ventilating appropriately, if they are acidotic or alkalotic, and now, diagnosing our patients as being septic.
Historically speaking, EMS providers have not always been very good at diagnosing sepsis, so treatments have been delayed or withheld, worsening our patients’ outcomes. After a patient begins displaying signs of sepsis, their mortality rates will increase about 8 percent, for every hour that treatment is withheld. But how have we traditionally diagnosed sepsis? The Quick Sequential Organ Failure Assessment score or qSOFA criteria has been the most common diagnostic tool for years. With qSOFA we were determining if our patient has a respiratory rate greater than 22 breaths per minute, an altered mental status, and a blood pressure less than 100 systolic. But there are a lot of things that can cause a higher respiratory rate, lower blood pressure, and an altered mental status; this is what makes diagnosing sepsis in the field so difficult. Usually when people get sick, they develop a fever, and this was usually our first clue that they could be septic, but checking a temperature isn’t even part of the qSOFA criteria, because sometimes they are febrile, and sometimes they aren’t. So, we think, no fever, no infection, no sepsis… this thinking has led us to misdiagnosing and delaying vital treatment.
 In the EMS setting, most of us don’t have the ability to draw labs, we don’t have ultrasound, x-rays, CTs or MRIs, etc., so we tend to miss some things, sepsis should not be one of those things. Now enter ETCO2. Since most of us cannot draw labs, we need some other diagnostic tool to help us. “ETCO2 had a higher discriminatory power to predict mortality, sepsis, and severe sepsis than qSOFA.” (EB Medicine, 2021).
In the EMS setting, most of us don’t have the ability to draw labs, we don’t have ultrasound, x-rays, CTs or MRIs, etc., so we tend to miss some things, sepsis should not be one of those things. Now enter ETCO2. Since most of us cannot draw labs, we need some other diagnostic tool to help us. “ETCO2 had a higher discriminatory power to predict mortality, sepsis, and severe sepsis than qSOFA.” (EB Medicine, 2021).
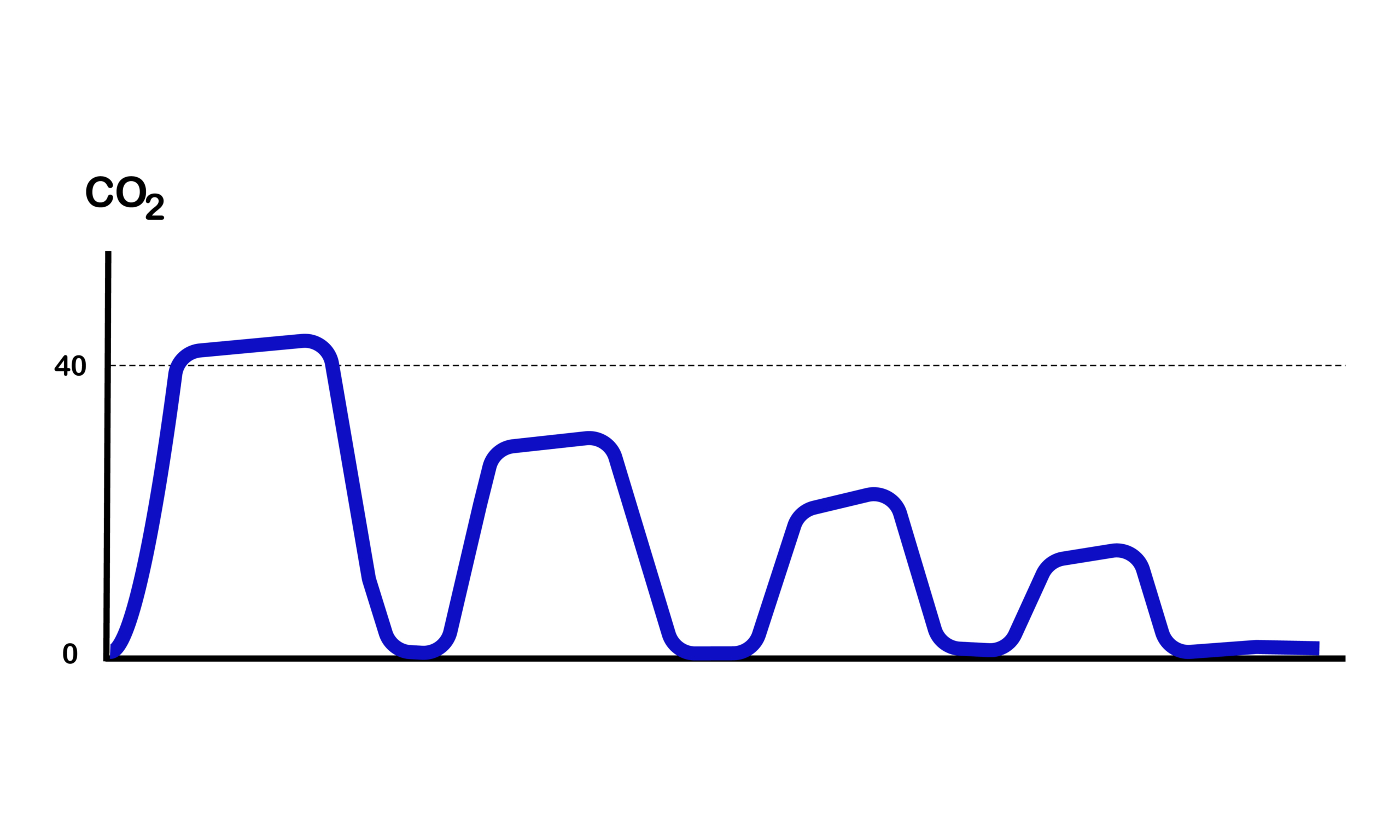
A normal ETCO2value for a healthy person should be between 35-45 mmHg. We have seen that a decrease in this value, could indicate several things, such as hypoperfusion, certain dysrhythmias, and even sepsis. When a person becomes septic, their body is working very hard to try to heal itself, causing a rise in their lactate (lactic acid) levels, leading to metabolic acidosis. The increase in their body’s acidity levels, causes an increase in their respiratory rate because their body wants to get rid of that excess acid, and get back into a state of homeostasis. As the respiratory rate increases, this causes the patient to breathe off excess carbon dioxide, decreasing the ETCO2 number. The higher their lactate levels go, the lower their CO2 levels go.
“Early identification of sepsis significantly improves outcomes, suggesting a role for prehospital screening. An end-tidal carbon dioxide (ETCO2) value ≤ 25 mmHg predicts mortality and severe sepsis when used as part of a prehospital screening tool.” (West J Emerg Med., 2018 May).
Knowing this information, it doesn’t matter if you are able to draw labs or not, it does not truly matter if the patient has a fever or not, we know that if there is any possibly that the patient could be sick or have some type of infection, they have a higher than normal respiratory rate, and a lower ETCO2, they are likely septic and you need to start treating that right away to try to improve the patients chance of having a good outcome.
References: