While many may view HEMS organizations as a specialty unto itself many programs have true specialized teams for certain populations. One can think of HEMS providers as a jack of all trades but generally a master of none. We care for all patient populations a health system can see, from the earliest of premature babies to the elderly to the bariatrics. We handle ECMO patients, ballon pumps, impelas, VADS, and organ transfers. But for the most part we handle these populations and the specialty equipment at the surface level. For the times where the benefits outweigh the costs as well as the risks, we should utilize the specialists to help in the transport. Some of these specialists should include, NICU providers (NP, RT, NICU RN), high risk pregnancy team, perfusionists, and field surgical teams.
Lets start by discussing the NICU teams. To define this better, these are single providers or a team of providers that supplement a flight crew as opposed to independent children’s transport teams. When a program focuses on training and education related to the care of newborns the use of independent NICU providers can essentially be limited to the sickest or most complex babies. With this specific sub set of medicine ventilation and oxygenation tend to be the most important aspect of care and while standard ventilated NICU patients shouldn’t be concerning for flight providers there are extensive non-standard ventilation modes and strategies which would benefit from a specialist to manage ventilation and oxygenation. Some examples of this would be, inverse ratio ventilation strategies (IRV), high frequency ventilation, and neurallyadjusted ventilatory assist (NAVA). In many cases transporting a patient who is ventilated with one of these advanced modes may not even be possible and a specialty team would be helpful in switching the patient to a more “normal” mode of ventilation. When are these specialty providers not needed? They should not be used for standard HFNC, Bi-Pap patients, or standard modes of ventilation. One of the most difficult parts in the utilization of these teams is the involvement or lack of involvement from program leadership, vs policy, vs an operations or communications center understanding of the situation, essentially how and when do we utilize the providers. The below table is a proposed example of a guideline which could be helpful in determining when a specialty provider should go.
|
Age |
Vital Signs |
Airway |
Vent Mode |
Team |
|
<37 Weeks |
MAP <gestational age despite 1 pressor Stable MAP |
Controlled Uncontrolled |
Standard Non-Standard |
NP / NICU RN RT Standard Flight team |
|
37-week – term |
MAP unstable despite 1 pressor (possible but in the absence of other factors flight crew should handle) Stable MAP |
Controlled Uncontrolled |
Standard Non-standard |
NP / NICU RN RT Standard Flight team |
|
Term- 1 month of life |
Unstable MAP with 1 pressor Stable MAP |
Controlled Uncontrolled(possible depending on known or suspected abnormalities) |
Standard Non-Standard |
NP / NICU RN RT Standard Flight team |
*Please note there is no research to support this proposed guideline, direction should ultimately rest with the program and NICU medical director.*
Any program utilizing specialty providers on the aircraft or even on ground assetsassumes the responsibility for their safety. Programs are responsible for their initial orientation as well as yearly competency training. These providers should have a crew resource management class, standard aircraft orientation completed by the pilot in command, a minimum of 2 weeks of flying as a third provider, along with PALS.
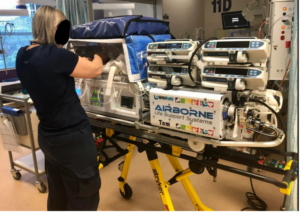
Perfusionist and high-risk OB teams would follow the same generalized approach. Due to the cost of training and remaining proficient as a nurse qualified to run an ECMO machine it is very cost prohibitive to have all the nurses in a program trained. Therefore, a perfusionist should accompany the ECMO circuit. These providers should be screened, trained and integrated into the flight team in the same manner as a NICU provider or team member.
The field surgical team while an extremely rare asset to need is a vital part of bringing prehospital care to the entrapped patient. While this may seem to be a once in a career type of incident there has been at least three occasions even within my own county or first due area where a physician has been needed to respond for a field amputation. Once we realize the patient is extensively trapped is not the time to try and find a doctor to perform an impromptu amputation. These are regionalized specialty teams that EMS systems at the state level should have preestablished. One excellent example of this is the University of Maryland Shock Trauma’s Go-Team. The team is made up of one attending physician (anesthesia, surgery, or critical care) and a CRNA . These specialty teams are trained to provide care in austereenvironments such as confined space, building collapses, high angle, farm, and water rescues scenarios. In general we want to ensure that we are calling for and utilizing these resources appropriately, we should consider the time it will take to extricate a patient or if extrication is possible. Anytime extrication is unlikely or it will take over an hour to complete the extrication (along with some type of serious injury such as an impalement, or crush injury) these specialty teams may be your best option for helping to manage the patient over this long process.
In conclusion we want to make sure that we are managing risks and costs while still doing the right thing for our patients in regards to the utilization of specialty teams. Anytime we bring people under the rotor disk we assume the risk of an accident whether its actually loading or unloading the aircraft, responding to the scene, or returning from a flight what we do as flight providers has inherent risks. But along with risk also comes costs. Many times, we are adding additional legs to these flights in order to pick up specialty teams. For instance, according to airbus the average cost to operate a EC145 per hour is 2,300 dollars (assumes a 6$ per gallon fuel cost). Along with the per hour cost in many instances only a medium sized aircraft like a EC145 or an Augusta 139/169 will be capable of routinely being able to fit and lift the added crew and equipment needed for these specialty teams. This only drives the programs costs up for providing these services. However, there is no substitute for these specialty teams when they are truly needed and as such, we as critical care providers must remain integral in properly utilizing these resources.