Predicting the difficult airway is a combination of art and science. Sometimes the airway that looks relatively easy to manage can turn out to be a nightmare and the supposedly difficult airway based on external assessment can be managed relatively simple to maintain.
A good rule of thumb is to always hope for the best while preparing for the worst. This approach allows the provider to have multiple back up options in the event that the airway proves difficult if not almost impossible to manage. There are many different acronyms that aid the healthcare provider in assessing and anticipating the difficult airway.
The MOANS and BEARD acronym are memory aids to predict a patient that may be difficult to ventilate with a bag valve mask.
MOANS stands for:
M=Mask Seal (Think beard, blood and/or anatomic variances)
O=Obesity/Obstruction (Both might make performing a patent mask seal difficult to obtain) A=Age (Extremes of Age can make obtaining a consistent mask seal difficult)
N=No Teeth (Lack of teeth or facial structures leave the provider with no support against which the mask can form a patent seal against)
S=Stiff Lungs/Apnea (Overcoming the resistance of stiff lungs works against the provider’s ability to provide a good mask seal and adequate tidal volumes)
BONES stands for:

B=Beard (Again facial hair can make obtaining a good mask seal difficult) O-Obesity (Excessive body habitus makes positioning difficult)
N=Neck Stiffness (Can make it difficult to adequately displace the tongue and open the airway) E=Elderly (Elderly patients may have a kyphotic spine and also have a tendency to decompensate more rapidly than their younger counterparts)
S=Snoring/Sleep Apnea (Again, this condition can make maintaining a patent airway and providing adequate tidal volumes difficult)
The acronym RODS is used to predict a difficult supraglottic or extraglottic airway device placement and utilization

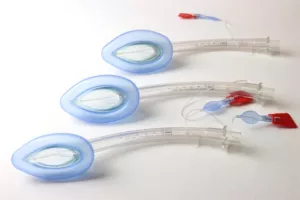

R=Restricted Mouth Opening (May make insertion of extraglottic/supraglottic airway device into the oral cavity difficult
O=Obstruction (Any airway narrowing or deformity can make placing these devices difficult) D=Disrupted/Distorted Airway (As above, this can make placing and maintaining the proper placement of a supraglottic/extraglottic device more difficult)
S=Stiff Lungs/Spinal Immobilization (The combination of stiff lungs and limited spinal mobility due to immobilization devices can make placing and maintaining airway patency with a supraglottic/extraglottic device a challenge)
When it comes to orotracheal intubation, there are two widely accepted acronyms to assist in predicting the difficult intubation.
HEAVEN stands for:
H=Hypoxemia (Hypoxemia may cause the patient to desaturate rapidly and irreversibly) E= Extremes of Size (As above can make the advanced airway instrumentation difficult) A=Anatomy Challenges (Absent or abnormally shaped anatomy can make airway structure identification difficult if not impossible)
V=Vomit, Blood, Fluid (Any foreign substance can increase the risk of aspiration pneumonia or pneumonitis and make visualization of airway structures hard to identify)
E-Exsanguination (Blood Loss can increase the rate and severity of desaturation)
N=Neck Mobility (Limited Neck Mobility can make performing an effective head tilt/chin lift almost impossible, which can in turn limit airway patency and visualization)
LEMON stands for:
L=Look Externally (Look for any outward difficult airway management clues)
E=Evaluate the 3-3-2 rule
(3 of the patients fingers from upper to lower incisors)
(3 of the patients finger breadth from the tip of the chin to to the hyoid bone)
(2 of the patients finger breadth from the angle of the jaw to the thyroid cartilage)
M=Mallampati Scale (Uvula is the focus)
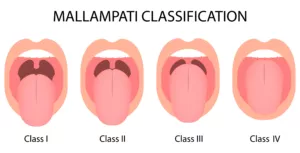
Mallampati I: (ability to visualize the posterior pharynx, and all of the uvula)
Mallampati II: (The posterior pharynx is partially exposed and most of the uvula is seen)
Mallampati III: (Only part of the soft palate and the base of the uvula are able to be visualized)
Mallampati IV: (No posterior structures can be seen, nor can the uvula be seen) O=Obstruction/Obesity (These can make positioning a patient for successful first pass success less likely)
N=Neck Mobility (Limited neck mobility works against the normal positioning to allow for better visualization of important airway landmarks)
As you can see, there are many tools available to assist the healthcare provider with predicting the potential difficult airway. Once a difficult airway is suspected, the prudent provider must weigh the benefits and risks of each airway management modality. Sometimes simpler is better than more complex interventions as long as no further harm is done and the patient can be managed with less invasive techniques until additional help or resources are on hand.

