Utilizing invasive hemodynamic monitoring utilizing an arterial line has both advantages and risks that healthcare providers need to be aware of. While it offers the ability to monitor real time beat to beat changes in perfusion status, it also has potential complications that non invasive monitoring devices do not have. All prehospital providers should be familiar with the standard vital signs including heart rate, ventilatory rate, blood pressure, oxygen saturation and end tidal carbon dioxide monitoring. Arterial line monitoring however, is a monitoring modality that many providers are somewhat unfamiliar, if not completely uncomfortable with. In the following article, we will discuss the risks and benefits of invasive hemodynamic monitoring in the inter facility and critical care environments.
Standard blood pressure monitoring frequently involves auscultation of a systolic and diastolic blood pressure using a blood pressure cuff and stethoscope. Blood pressure readings can vary widely based on ambient noise levels, cuff size and location, stethoscope quality, regularity of the pulse rate and overall hearing acuity of the provider. Listening for the beginning of the audible heart beat as the cuff manometer gauge slowly trends down (Systolic) and when that heart beat again disappears (Diastole) gives us our blood pressure reading. With invasive hemodynamic monitoring, these variables are largely taken out of the equation. Additionally, non invasive blood pressures tend to under read at higher pressures and over read at lower pressures. This can lead to over or under treating of our patients based on perceived perfusion status gleaned from auscultation of non invasive blood pressures. Noisy environments may necessitate obtaining a blood pressure by palpation. This method only provides us with a systolic blood pressure reading. As with any vital sign parameter, we should use each vital sign as a piece of the puzzle and not as a be all to end all decision making tool that guides our treatment decisions. Non invasive blood pressures are often taken every 5-15 minutes based on the providers’ impression of how sick our patient is, whereas arterial line monitoring gives us a continuous accurate beat to beat assessment of the patient’s perfusion status. The immediate effects of interventions can often be seen more accurately and rapidly than with a non invasive blood pressure. Think of a standard blood pressure assessment as a snap shot at a point in time, while arterial lines are more like a movie or video in real time. Arterial lines also allow the provider to obtain ABG’s (arterial blood gas) analysis, but do not offer the ability to administer fluids or medications via the arterial line route.
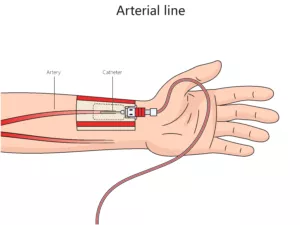
Invasive hemodynamic monitoring via an arterial line is not without its potential complications and risks. First off, once an arterial line is placed in an artery (often the femoral or radial artery), all perfusion distal to the insertion site is potentially at risk due to arterial occlusion. This is why prior to placing a radial arterial line an Allen Test is performed to confirm adequate collateral circulation to the distal hand in the event of radial artery occlusion from the catheter itself. Infection is always a risk anytime a device crosses from the exterior to the interior regions of the body. Central Line Associated Blood Stream Infection (CLABSI) and Catheter Related Blood Stream Infection (CRBSI) are one of the most frequent complications related to in dwelling arterial lines and often result in longer hospital stays. Inadvertent dislodgment during transport can have devastating consequences if left unrecognized during transport. Unrecognized bleeding from a dislodged arterial line catheter can bleed out within minutes. Additionally, setting up arterial line can be an intimidating ordeal for the provider that is unfamiliar with the proper set up and priming of an invasive arterial line device. Like any other intervention or assessment modality, frequent use and troubleshooting will improve the confidence level of the person utilizing the device. When changes in barometric or atmospheric pressures is encountered as with non pressurized rotorcraft flight, the arterial line must be “zeroed” to atmosphere to avoid inaccurate readings. These inaccurate readings can lead to errors in treatment based on arterial line reading deviations.
While there are many advantages to invasive hemodynamic monitoring, there are many potential risks that the provider needs to be aware of. Proper utilization can lead to rapid recognition of both improvements and deteriorations of our patient’s perfusion status. Accurate arterial line monitoring can guide our treatment decisions more effectively than non invasive blood pressure readings, especially when administering vasopressors or catecholamines. As with any monitoring device or piece of medical equipment, there are always advantages and disadvantages/risks. Knowledge of the how to maximize the advantages and minimize/recognize the disadvantages/risks can go a long way towards improving the overall care we provide to our sickest patients. While this monitoring modality may not currently be in your specific tool box or scope of practice, knowledge of the basic pros and cons of using this device will allow you to improve your patient care either now or in the future.
