“When faced with managing the airway of the pregnant patient, it is important to understand the anatomic and physiologic changes that occur during gestation. Not only does the pregnant female have to oxygenate, ventilate, perfuse and nourish the developing fetus, specific anatomic changes occur due to hormonal changes and fluctuations due to pregnancy. Often, intubation and aggressive, yet appropriate, airway management is delayed due to the provider’s lack of comfortability with managing and securing the airway of the pregnant patient.
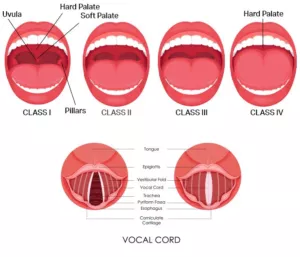
Pregnant females tend to desaturate and decompensate more rapidly than their non- pregnant counterparts due to a variety of factors. Pregnancy is associated with general weight gain and increase in breast size which can make airway device insertion more difficult. The increase in circulating progesterone levels can increase the tissue vascularity which can increase the likelihood of soft tissue bleeding during instrumentation. Mallamapati scores can increase by 1 to 2 grades during gestation making airway structure visualization more difficult.
Functional Residual Capacity decreases during pregnancy due to the displacement of the diaphragm by the gravid uterus. This can lead to shorter periods of safe apnea despite effective pre oxygenation and nitrogen washout. Nothing can stress out a healthcare provider more than witnessing a desaturating patient while attempting to manage their airway. Normal fetal development can increase the metabolic demands on the mother which in turn can increase Minute Ventilation requirements.

Hormonal fluctuations can also relax smooth muscles of the upper epigastric sphincter which in turn can increase the likelihood of vomiting. If not treated appropriately and promptly, this can lead to aspiration and the complications associated with it.
So how do we manage these patients? First off, be prepared for conditions like desaturation and vomiting. Aggressively pre oxygenate the patient, have suction hooked up, running and readily available. Position the patient so that the three airway axis are as aligned as possible. Often this is accomplished by placing the patient in the “sniffing position” or ramping the patient. If available, utilize video laryngoscopy to increase your first pass success rate during intubation. Respect the fact that your patient will more often than not desaturate more rapidly during airway instrumentation so make sure that all primary and secondary airway devices are within reach and ready to be deployed. Intubate earlier instead of later because once deterioration begins, it usually will progress faster in the obstetric patient than it will in the non pregnant female. Position the patient BEFORE any airway maneuvers are attempted to decrease that period of apnea and to decrease the chances of airway contamination. Any unprotected airway is at an increased risk of contamination so anything we can do to decease that time frame will in turn decrease the likelihood of aspiration. Keep in mind that normal gestational changes often result in increased minute ventilation requirements so a high end normal minute ventilation calculation is something to consider. Recent studies have shown that intubation carries I higher discomfort level than the actual surgical procedure itself.
If possible, make sure the patient is adequately sedated and/or paralyzed during intubation attempts to decrease the amount of distress that often accompanies airway instrumentation.
Understanding the physiologic and anatomic changes that occur during pregnancy coupled with a high index of suspicion for rapid desaturation and decompensation can improve patient outcomes when managing the obstetrical airway. Hoping for the best while preparing for the worst and being proactive in managing deterioration will assist the critical care/ prehospital provider in the care of the pregnant patient. Thankfully we don’t frequently have to aggressively manage the obstetrical airway, but when we are called to do so, seconds count.”

